Understanding Diverticulitis
Diverticulitis is a condition that affects many individuals, especially in the latter part of life. In this comprehensive overview, we will delve into the symptoms, diagnosis, and lifestyle management associated with diverticulitis.
Key Takeaways
- Diverticulitis occurs when small pockets in the colon become inflamed.
- Common symptoms include abdominal pain, fever, and changes in bowel habits.
- Diagnosis usually involves imaging tests and symptom analysis.
- A balanced diet and proper hydration are crucial for management.
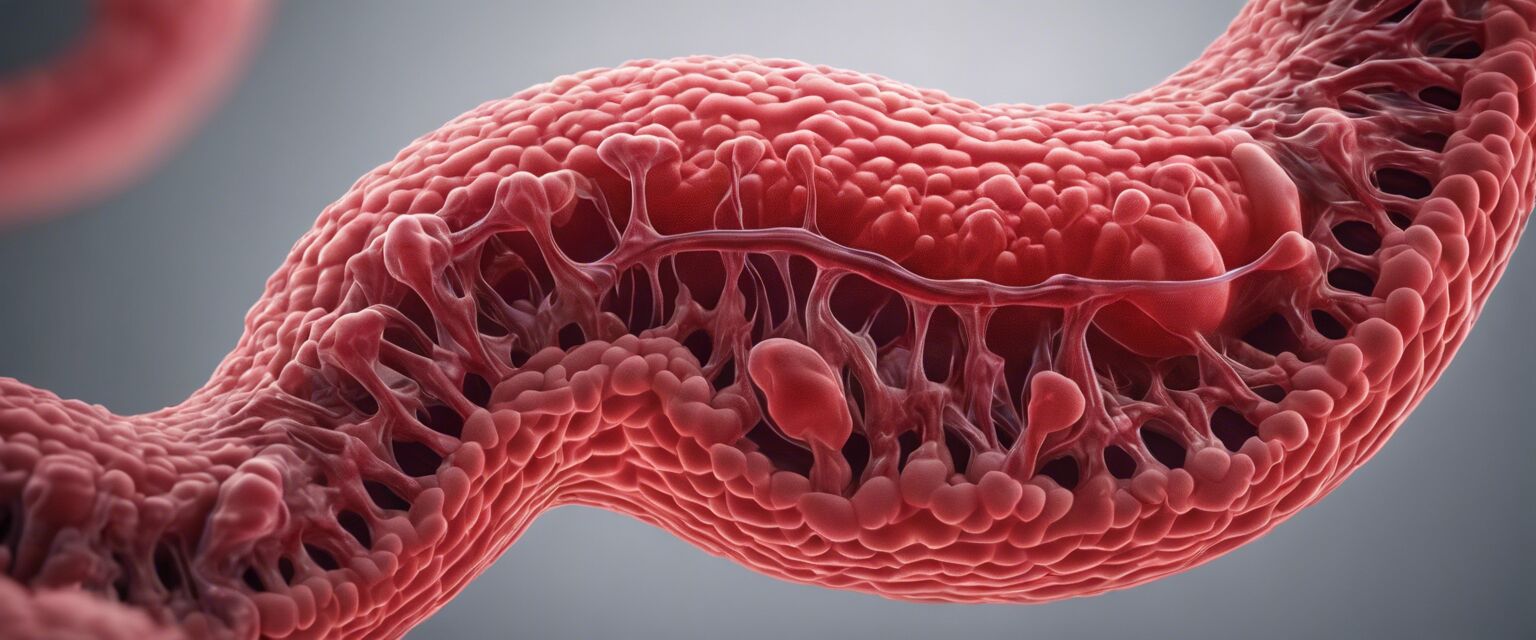
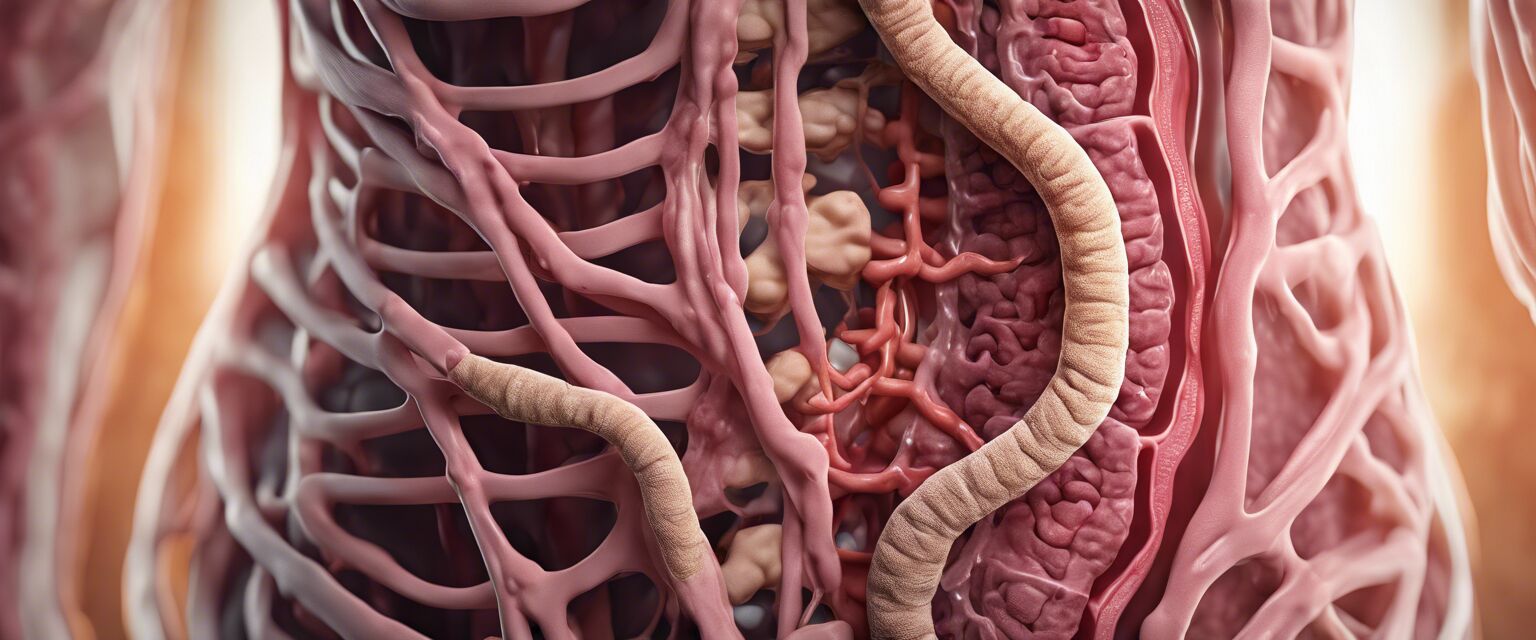
What is diverticulitis?
Diverticulitis is a gastrointestinal condition characterized by inflammation or infection of small pouches that can form in the walls of the digestive tract, specifically the colon. These pouches are known as diverticula. When these diverticula become inflamed, it leads to diverticulitis, which can cause abdominal pain and other symptoms.
Symptoms of diverticulitis
The signs and symptoms of diverticulitis can vary but generally include:
- Severe abdominal pain, often on the left side
- Fever
- Nausea and vomiting
- Changes in bowel habits (diarrhea or constipation)
- Bloating and gas
When to seek medical attention
If you experience persistent abdominal pain, fever, or have concerns about your digestive health, it is advisable to consult a healthcare professional. Early diagnosis and management are crucial.
Diagnosis of diverticulitis
Diagnosis of diverticulitis involves a combination of medical history, physical examination, and imaging tests. While doctors may perform a physical exam to check for tenderness in the abdomen, imaging studies provide clearer insights. Some common tests include:
| Test | Description |
|---|---|
| CT Scan | A imaging test that provides detailed images of the colon to assess inflammation. |
| Ultrasound | A rather non-invasive way to visualize the colon and check for infection. |
| X-ray | A less common method but can be used to identify complications. |
Management and treatment options
Managing diverticulitis can involve dietary modifications, medications, and in some severe cases, surgical intervention. Here's how these options can be classified:
Dietary modifications
Individuals with diverticulitis are often advised to follow a high-fiber diet to enhance bowel health. Adequate hydration is equally important to help prevent constipation.
Tips for managing diverticulitis
- Increase fiber intake through fruits, vegetables, and whole grains.
- Stay hydrated by drinking plenty of water daily.
- Limit red meat and processed foods.
- Avoid foods that can lead to bloating, such as carbonated beverages.
Medications
Your healthcare provider may prescribe medications to help manage pain or fight infection. It's essential to adhere to the prescribed treatments.
Table summarizing dietary recommendations
| Food Type | Examples |
|---|---|
| High-fiber foods | Fruits, vegetables, and whole grains |
| Healthy fats | Nuts, seeds, and avocados |
| Hydration | Water, herbal teas, and clear broths |
Surgical options
In recurrent or complicated cases, surgery may be necessary to remove the affected part of the colon. Always consult a healthcare provider to weigh the risks and benefits.
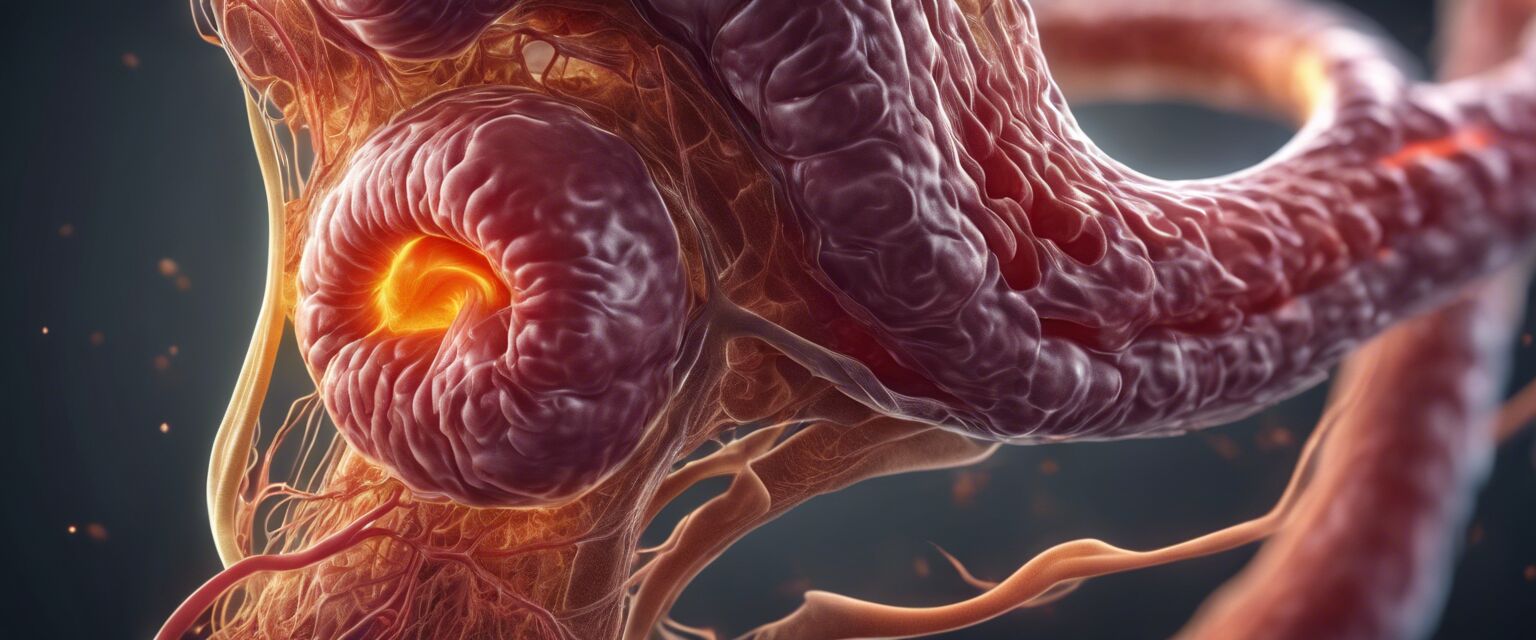
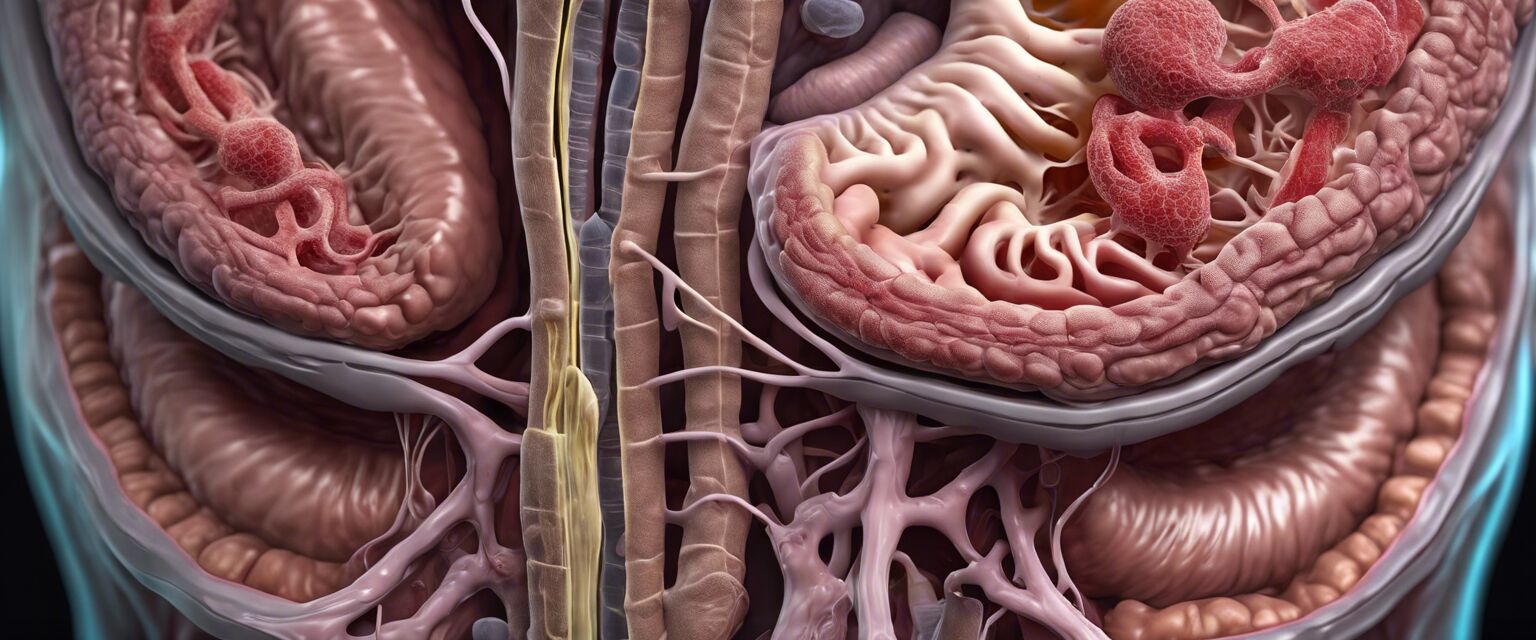
Complications of diverticulitis
If left untreated, diverticulitis can lead to serious complications, including:
- Abscesses in the abdomen
- Perforation of the colon
- Peritonitis
- Bowel obstruction
Living with diverticulitis
While diverticulitis can be a challenging condition, many individuals manage it effectively with lifestyle changes. Regular check-ups and maintaining a healthy diet play a significant role.
Resources for support
For more information and resources, check out our detailed guides on:
- Digestive health supplements
- Comfortable clothing
- Educational resources
- Stress management tools
- Specialized diet plans
Conclusion
Understanding diverticulitis is crucial for effective management. By recognizing symptoms early, seeking proper care, and making dietary adjustments, individuals can lead a healthy lifestyle despite the challenges posed by this condition.
Pros
- Effective management through dietary modification.
- Helpful medications for symptom relief.
- Supportive resources available for education.
Cons
- Can lead to severe complications if untreated.
- Chronic condition may require ongoing management.
- Diet restrictions may be challenging to maintain.